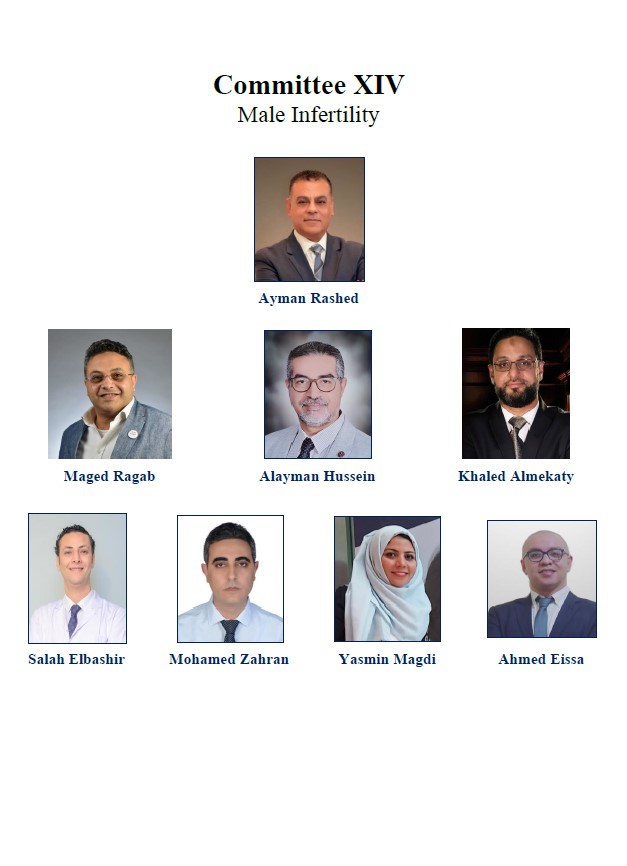
Committee XIV
Male Infertility
Prof. Ayman Rashed, MD, PhD, Professor of Urology, 6th October University, Cairo, Egypt
Prof. Maged Ragab, MD, PhD,Professor of Urology, Urology Department, Tanta University, Tanta, Egypt
Prof. Alayman Hussein, MD, PhD,Professor of Urology, Urology Department, Minya University, Minya, Egypt
Assis. Prof. Khaled Almekaty, MD, PhD,Assistant Professor of Urologt, Tanta University, Tanta, Egypt
Dr. Salah Elbashir, MD, PhD,Lecturer of Urology, Urology Department, Benha University, Benha, Egypt
Dr. Mohamed Zahran, MD, PhD,Lecturer of Urology, Urology Department, Mansoura University, Mansoura, Egypt
Dr. Yasmin Magdi, PhD,Consultant of Gynecology, Al-Yasmeen Fertility and Gynecology Center, Benha, Egypt
Dr. Ahmed Eissa, MD,Assistant Lecturer of Urology, Tanta University, Tanta, Egypt
Contents
- XIV.1 List of Abbreviations
- XIV.2 Abstract
- XIV.3 ASSESSMENT OF MALE INFERTILITY
- XIV.4 Evaluation of male infertility
- XIV.5 VARICOCELE
- XIV.6 AZOOSPERMIA
- XIV.7 POST- PUBERTAL CRYPTORCHIDISM
- XIV.8 MALE HYPOGONADISM
- XIV.9 ART AND MALE INFERTILITY
- XIV.10 REFERENCES
XIV.1 List of Abbreviations
- ARTs - Assisted Reproductive Techniques
- AZF - Azoospermia Factor Gene
- CBAVD - Congenital Bilateral Absence Of Vasa
- CFTR gene - Cystic Fibrosis Transmembrane Conductance Regulator gene mutation
- DFI - Defragmentation Index
- EDO - Ejaculatory Duct Obstruction
- E2 - Estradiol
- FISH - Fluorescent In-Situ Hybridization
- GnRH - Gonadotropin Releasing Hormone
- hCG - Human Chorionic Gonadotropin
- HPG - Hypothalamo Pituitary-testis
- IVF - In vitro Fertilization
- ICSI - IntraCytoplasmic Sperm Injection
- ITT - Intra-Testicular Testosterone
- IUI - Intrauterine Insemination
- LH - Luteinizing Hormone
- MENA - Middle East and North Africa
- NOA - Non-Obstructive Azoospermia
- OATs - OAT Syndrome
- OA - Obstructive Azoospermia
- OAT - Oligo-Astheno-Teratozoospermia
- PGD - Pre-Implantation Diagnosis
- PGT - Preimplantation Genetic Testing
- ROS - Reactive Oxygen Species
- US - Ultrasound
- SERM - Selective Estrogen Receptors Modulators
- SCD - Sperm Chromatin Dispersion
- SCSA - Sperm Chromatin Structure Assay
- SDF - Sperm DNA fragmentation
- SRR - Sperm Recovery Rate
- ASRM - The American Society for Reproductive Medicine
- TT - Total Testosterone
- TRUS - Trans-Rectal Ultrasound
- YCMD - Y- Chromosome Microdeletion
XIV.2 Abstract
XIV.2.1 Objective
XIV.2.2 Methods
XIV.2.3 Results
XIV.2.4 Conclusions
XIV.3 ASSESSMENT OF MALE INFERTILITY
XIV.3.1 Definition and classification
XIV.3.2 Epidemiology
XIV.3.3 Etiology
- Increased scrotal temperature
- Hormonal disruption
- Environmental factors
- Congenital genital anomalies
- Genetic abnormalities
- Erectile dysfunction
- Genital infection
- Immunological factors
- Malignancy
- Idiopathic
Recommendation |
Strength Rating |
|---|---|
XIV.4 Evaluation of male infertility
XIV.4.1 Why to evaluate?
- Correctable diagnosed conditions.
- Irreversible conditions that are amenable to assisted reproductive techniques (ARTs).
- Irreversible conditions that is not amenable to treatment or ARTs, to save time and cost of unnecessary procedures. In such cases it is better to direct the treatment to other condition e.g. erectile dysfunction due to hypogonadism.
- Underlying life-threatening conditions that may presented by infertility (e.g. testicular tumor).
- Genetic abnormalities that may have impact on the offspring.
XIV.4.2 Timing of evaluation?
XIV.4.3 Medical history
- Duration of infertility and if primary or secondary infertility.
- Partner age and relevant history.
- Sexual history including (erectile function, intercourse rate, ejaculatory disorders, STDs)
- Childhood relevant diseases (e.g. mumps orchitis) and developmental and pubertal history (e.g. undescended testes, hypospadias, …etc.)
- Gonadotoxins exposure e.g. chemotherapy, radiotherapy, medications, heat, ...etc.
- Systemic medical diseases (e.g.,DM, dyslipidemia and upper respiratory diseases)
- History of previous relevant surgeries e.g. herniorrhaphy, varicocelectomy, hydrocelectomy, urethral surgery, abdomino-perineal surgery, …etc.
XIV.4.4 Physical examination
XIV.4.4.1 General Examination
- Scars of relevant previous operations
- General facies status of the patient
- Hair distribution
- Body proportion and fat distribution
- Gynecomastia
- Any apparent congenital anomalies
XIV.4.4.2 Local Examination
- Penile examination for size and position of external meatus
- Scrotal examination for development of scrotal sac, and size and consistency of both testes, examination of epididymis and vasa differentia, and examination for varicocele, hydrocele or masses
XIV.4.5 Laboratory investigations
Parameter |
Lower reference limit |
|---|---|
XIV.4.5.1 Semen Analysis
XIV.4.5.2 Semen cryopreservation
XIV.4.5.3 Sperm DNA fragmentation (SDF) test
- Sperm chromatin structure assay (SCSA), (n = < 30%)
- Terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick end labeling (TUNNEL), (n = < 12%)
- Single cell gel electrophoresis (SCGE or COMET) (n= < 25%)
- Sperm Chromatin Dispersion (SCD) (n = Large chromatin halo dispersion around the sperms)
- Unexplained Infertility
- Recurrent pregnancy loss either spontaneous or after IVF/ICSI
- Recurrent IUI failure
- Borderline abnormal or normal semen analysis with risk factors (e.g. clinical varicocele, smoking, poor lifestyle, exposure to gonadotoxins, etc).
XIV.4.6 Hormonal evaluation
- Subfertile semen analysis particularly if count < 10 mil/cc
- Associated sexual dysfunction
- Clinical conditions that suggest endocrinopathy
XIV.4.7 Genetic tests
- Finalizing the diagnosis of infertility problem.
- The risk of passing genetic problems to offspring.
- Saving money and time if the male infertility due to untreatable genetic problems e.g. XX male
XIV.4.7.1 Indications for Genetic testing:
- Suspected obstructive azoospermia (OA)
- Patients with sperm count < 10 mil/cc
- Severe oligozoospermia (< 5 mil/cc), particularly, in patients, who did not show any documented sperm count above 5 mil/cc.
- In cases of sexual differentiation disorders
- Patients with high FSH, low TT, and low testicular volume
- Apparent facial or body disconfiguration, or known congenital disorder relevant to male infertility (e.g. patients with, polycystic kidney disease, Prader-Willi Syndrome, Noonan Syndrome, etc.)
- Recurrent miscarriage and/or recurrent failure of ARTs.
- Recurrent failure of TESE/mTESE.
XIV.4.7.2 Basic Genetic Testing in Male Infertility:
XIV.4.8 Imaging
XIV.4.8.1 Scrotal ultrasound (US)
Recommendation |
Strength Rating |
|---|---|
XIV.5 VARICOCELE
XIV.5.1 Definition
XIV.5.2 Incidence
XIV.5.3 Diagnosis and classification
- Grade I varicocele (palpable with Valsalva maneuver)
- Grade II (palpable at rest, but not visible)
- Grade III (varicocele visible without palpation).
XIV.5.4 Management
Recommendation |
Strength Rating |
|---|---|
XIV.6 AZOOSPERMIA
XIV.6.1 Assessment of Azoospermia patients
Recommendation |
Strength Rating |
|---|---|
XIV.6.2 Further assessment of Azoospermic patients
Recommendation |
Strength Rating |
|---|---|
Recommendation |
Strength Rating |
|---|---|
XIV.6.3 Management of Azoospermia
XIV.6.4 Idiopathic male infertility and Oligo-astheno-teratozoospermia (OAT)
- Empirical treatments
- Life-style modification (weak recommendation)
- Weight loss (weak recommendation)
- Physical activity (weak recommendation)
- Smoking cessation (weak recommendation)
- Alcohol consumption (weak recommendation)
- Antioxidant treatment: oxidative stress may induce idiopathic infertility, so antioxidant may show a response in treatment of Idiopathic Male Factor Infertility (weak recommendation)
- Idiopathic Male Factor Infertility
Recommendations |
Strength Rating |
|---|---|
Recommendations |
Strength Rating |
|---|---|
XIV.7 POST- PUBERTAL CRYPTORCHIDISM
Recommendations |
Strength Rating |
|---|---|
XIV.8 MALE HYPOGONADISM
XIV.8.1 Introduction
XIV.8.2 Definition and epidemiology
Recommendations |
Strength Rating |
|---|---|
XIV.8.3 Evaluation of hypogonadal men
Recommendations |
Strength Rating |
|---|---|
XIV.8.3.1 Management of infertile men with hypogonadism
XIV.8.3.2 Human chorionic gonadotropin (hCG)
XIV.8.3.3 Selective estrogen receptors modulators (SERM):
XIV.8.3.4 Non-steroidal aromatase inhibitors (Anastrozole and Letrozole):
Recommendations |
Strength Rating |
|---|---|
XIV.9 ART AND MALE INFERTILITY
XIV.9.1 Introduction
XIV.9.2 Intrauterine insemination (IUI)
Recommendations |
Strength Rating |
|---|---|
XIV.9.3 In vitro fertilization (IVF)
Recommendations |
Strength Rating |
|---|---|
XIV.9.4 Intracytoplasmic sperm injection (ICSI)
Recommendations |
Strength Rating |
|---|---|
XIV.9.5 Preimplantation genetic testing (PGT)
Recommendations |
Strength Rating |
|---|---|
XIV.10 REFERENCES
2. Skakkebæk NE, Jørgensen N, Main KM, Meyts ER De, Leffers H, Andersson AM, et al. Is human fecundity declining? Int J Androl 2006; 29:2–11. https://doi.org/10.1111/j.1365-2605.2005.00573.x.
3. Elbardisi H, Majzoub A, Al Said S, Al Rumaihi K, El Ansari W, Alattar A, et al. Geographical differences in semen characteristics of 13 892 infertile men. Arab J Urol 2018; 16:3–9. https://doi.org/10.1016/j.aju.2017.11.018.
4. Eldib A, Tashani O. Infertility in the Middle East and North Africa Region: A systematic review with meta-Analysis of prevalence surveys. Libyan J Med Sci 2018; 2:37. https://doi.org/10.4103/ljms.ljms_24_18.
5. Nieschlag E, Hermann M. Behre, Nieschlag S. Andrology. 3rd ed. Springer; 2010.
6. Jarow J, Sigman M, Kolettis PN, Lipshultz LR, Mcclure RD, Nangia AK, et al. The Optimal Evaluation of the Infertile Male : AUA Best Practice Statement. Am Urol Assoc Educ Res Inc 2010:1–38.
7. Pfeifer S, Butts S, Dumesic D, Fossum G, Gracia C, La Barbera A, et al. Diagnostic evaluation of the infertile male: A committee opinion. Fertil Steril 2015;103: e18–25. https://doi.org/10.1016/j.fertnstert.2014.12.103.
8. Salonia A, Bettoocchi C, Carvalho J, Corona G, Minhas S, Serefoglu EC. EAU Guidelines on Sexual and Reproductive Health 2020:10–31. https://uroweb.org/guideline/sexual-and-reproductive-health/.
9. WHO. WHO | WHO laboratory manual for the examination and processing of human semen 2010. https://www.who.int/reproductivehealth/publications/infertility/9789241547789/en/ (accessed April 15, 2020).
10. Anger JT, Gilbert BR, Goldstein M. Cryopreservation of sperm: Indications, methods and results. J Urol 2003; 170:1079–84. https://doi.org/10.1097/01.ju.0000084820.98430.b8.
11. Han TS, Bouloux PMG. What is the optimal therapy for young males with hypogonadotropic hypogonadism? Clin Endocrinol (Oxf) 2010; 72:731–7. https://doi.org/10.1111/j.1365-2265.2009.03746.x.
12. Whitten SJ, Nangia AK, Kolettis PN. Select patients with hypogonadotropic hypogonadism may respond to treatment with clomiphene citrate. Fertil Steril 2006; 86:1664–8. https://doi.org/10.1016/j.fertnstert.2006.05.042.
13. Hussein A, Ozgok Y, Ross L, Rao P, Niederberger C. Optimization of spermatogenesis-regulating hormones in patients with non-obstructive azoospermia and its impact on sperm retrieval: A multicentre study. BJU Int 2013;111. https://doi.org/10.1111/j.1464-410X.2012.11485.x.
14. Shoshany O, Abhyankar N, Mufarreh N, Daniel G, Niederberger C. Outcomes of anastrozole in oligozoospermic hypoandrogenic subfertile men. Fertil Steril 2017; 107:589–94. https://doi.org/10.1016/j.fertnstert.2016.11.021.
15. Kim GY. What should be done for men with sperm DNA fragmentation? Clin Exp Reprod Med 2018; 45:101–9. https://doi.org/10.5653/cerm.2018.45.3.101.
16. Cho CL, Agarwal A, Majzoub A, Esteves SC. Clinical utility of sperm DNA fragmentation testing: Concise practice recommendations. Transl Androl Urol 2017;6:S366–73. https://doi.org/10.21037/tau.2017.07.28.
17. Cho CL, Agarwal A. Role of sperm DNA fragmentation in male factor infertility: A systematic review. Arab J Urol 2018; 16:21–34. https://doi.org/10.1016/j.aju.2017.11.002.
18. Elbashir S, Magdi Y, Rashed A, Ibrahim MA, Edris Y, Abdelaziz AM. Relationship between sperm progressive motility and DNA integrity in fertile and infertile men. Middle East Fertil Soc J 2018. https://doi.org/10.1016/j.mefs.2017.12.002.
19. Varghese AC, Tan G, Chan P, Tan SL. Clinical usefulness of sperm DNA fragmentation testing. Transl Androl Urol 2017;6: S484–7. https://doi.org/10.21037/tau.2017.06.12.
20. Panner Selvam MK, Agarwal A. A systematic review on sperm DNA fragmentation in male factor infertility: Laboratory assessment. Arab J Urol 2018; 16:65–76. https://doi.org/10.1016/j.aju.2017.12.001.
21. Practice Committee of the American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing: A guideline. Fertil Steril 2013; 99:673–7. https://doi.org/10.1016/j.fertnstert.2012.12.049.
22. Esteves SC, Roque M, Bradley CK, Garrido N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: systematic review and meta-analysis. Fertil Steril 2017; 108:456-467.e1. https://doi.org/10.1016/j.fertnstert.2017.06.018.
23. Ramasamy R, Lin K, Gosden LV, Rosenwaks Z, Palermo GD, Schlegel PN. High serum FSH levels in men with nonobstructive azoospermia does not affect success of microdissection testicular sperm extraction. Fertil Steril 2009; 92:590–3. https://doi.org/10.1016/j.fertnstert.2008.07.1703.
24. Krausz C, Escamilla AR, Chianese C. Genetics of male infertility: From research to clinic. Reproduction 2015;150: R159–74. https://doi.org/10.1530/REP-15-0261.
25. Hezavehei M, Sharafi M, Kouchesfahani HM, Henkel R, Agarwal A, Esmaeili V, et al. Sperm cryopreservation: A review on current molecular cryobiology and advanced approaches. Reprod Biomed Online 2018;37:327–39. https://doi.org/10.1016/j.rbmo.2018.05.012.
26. Wosnitzer MS. Genetic evaluation of male infertility. Transl Androl Urol 2014;3:17–26. https://doi.org/10.3978/j.issn.2223-4683.2014.02.04.
27. Carrell DT, Wilcox AL, Lowy L, Peterson CM, Jones KP, Erickson L, et al. Elevated sperm chromosome aneuploidy and apoptosis in patients with unexplained recurrent pregnancy loss. Obstet Gynecol 2003;101:1229–35. https://doi.org/10.1016/S0029-7844(03)00339-9.
28. Bieth E, Hamdi SM, Mieusset R. Genetics of the congenital absence of the vas deferens. Hum Genet 2020. https://doi.org/10.1007/s00439-020-02122-w.
29. Hall S, Oates RD. UNILATERAL ABSENCE OF THE SCROTAL VAS DEFERENS ASSOCIATED WITH CONTRALATERAL MESONEPHRIC DUCT ANOMALIES RESULTING IN INFERTILITY : LABORATORY , PHYSICAL AND RADIOGRAPHIC FINDINGS , AND THERAPEUTIC ALTERNATIVES. J Urol 1993;150:1161–4. https://doi.org/10.1016/S0022-5347(17)35714-2.
30. Augarten A, Yahav Y, Laufer J, Szeinberg A, Dor J, Mashiach S, et al. Congenital bilateral absence of vas deferens in the absence of cystic fibrosis. Lancet 1994;344:1473–4. https://doi.org/10.1016/S0140-6736(94)90292-5.
31. Ravel C, Berthaut I, Bresson JL, Stiffroi JP. Prevalence of chromosomal abnormalities in phenotypically normal and fertile adult males: Large-scale survey of over 10 000 sperm donor karyotypes. Hum Reprod 2006;21:1484–9. https://doi.org/10.1093/humrep/del024.
32. Egozcue S, Blanco J, Vendrell JM, García F, Veiga A, Aran B, et al. Human male infertility: Chromosome anomalies, meiotic disorders, abnormal spermatozoa and recurrent abortion. Hum Reprod Update 2000;6:93–105. https://doi.org/10.1093/humupd/6.1.93.
33. Parizot E, Dard R, Janel N, Vialard F. Down syndrome and infertility: what support should we provide? J Assist Reprod Genet 2019;36:1063–7. https://doi.org/10.1007/s10815-019-01457-2.
34. Corona G, Pizzocaro A, Lanfranco F, Garolla A, Pelliccione F, Vignozzi L, et al. Sperm recovery and ICSI outcomes in Klinefelter syndrome: A systematic review and meta-analysis. Hum Reprod Update 2017;23. https://doi.org/10.1093/humupd/dmx008.
35. Donker RB, Vloeberghs V, Groen H, Tournaye H, van Ravenswaaij-Arts CMA, Land JA. Chromosomal abnormalities in 1663 infertile men with azoospermia: the clinical consequences. Hum Reprod 2017;32:2574–80. https://doi.org/10.1093/humrep/dex307.
36. Vockel M, Riera-Escamilla A, Tüttelmann F, Krausz C. The X chromosome and male infertility. Hum Genet 2019. https://doi.org/10.1007/s00439-019-02101-w.
37. Rohayem J, Nieschlag E, Zitzmann M, Kliesch S. Testicular function during puberty and young adulthood in patients with Klinefelter’s syndrome with and without spermatozoa in seminal fluid. Andrology 2016;4:1178–86. https://doi.org/10.1111/andr.12249.
38. Krausz C, Hoefsloot L, Simoni M, Tüttelmann F. EAA/EMQN best practice guidelines for molecular diagnosis of Y-chromosomal microdeletions: State-of-the-art 2013. Andrology 2014; 2:5–19. https://doi.org/10.1111/j.2047-2927.2013.00173.x.
39. Lorenc T, Krupniewski L, Palczewski P, Gołębiowski M. The Value of Ultrasonography in the Diagnosis of Varicocele. J Ultrason 2016; 16:359–70. https://doi.org/10.15557/JoU.2016.0036.
40. Du J, Li FH, Guo YF, Yang LM, Zheng JF, Chen B, et al. Differential diagnosis of azoospermia and etiologic classification of obstructive azoospermia: Role of scrotal and transrectal US. Radiology 2010; 256:493–503. https://doi.org/10.1148/radiol.10091578.
41. Abdulwahed SR, Mohamed EEM, Taha EA, Saleh MA, Abdelsalam YM, Elganainy EO. Sensitivity and specificity of ultrasonography in predicting etiology of azoospermia. Urology 2013; 81:967–71. https://doi.org/10.1016/j.urology.2013.01.001.
42. Zavattaro M, Ceruti C, Motta G, Allasia S, Marinelli L, Di Bisceglie C, et al. Treating varicocele in 2018: current knowledge and treatment options. J Endocrinol Invest 2018; 41:1365–75. https://doi.org/10.1007/s40618-018-0952-7.
43. Clavijo RI, Carrasquillo R, Ramasamy R. Varicoceles: prevalence and pathogenesis in adult men. Fertil Steril 2017; 108:364–9. https://doi.org/10.1016/j.fertnstert.2017.06.036.
44. Levinger U, Gornish M, Gat Y, Bachar GN. Is varicocele prevalence increasing with age? Andrologia 2007; 39:77–80. https://doi.org/10.1111/j.1439-0272.2007.00766.x.
45. Akbay E, Çayan S, Doruk E, Duce MN, Bozlu M. The prevalence of varicocele and varicocele-related testicular atrophy in Turkish children and adolescents. BJU Int 2000; 86:490–3. https://doi.org/10.1046/j.1464-410X.2000.00735.x.
46. Baigorri BF, Dixon RG. Varicocele: A Review. Semin Intervent Radiol 2016; 33:170–6. https://doi.org/10.1055/s-0036-1586147.
47. Belay R, Huang G, Shen J-C, Ko EK. Diagnosis of clinical and subclinical varicocele: how has it evolved? Asian J Androl 2016; 18:182. https://doi.org/10.4103/1008-682X.169991.
48. Dubin L, Amelar RD. Varicocele Size And Results of Varicocelectomy in Selected Subfertile Men with Varicocele*. Fertil Steril 1970; 21:606–9. https://doi.org/10.1016/S0015-0282(16)37684-1.
49. Pfeifer S, Butts S, Catherino W, Davis O, Dumesic D, Fossum G, et al. Report on varicocele and infertility: A committee opinion. Fertil Steril 2014; 102:1556–60. https://doi.org/10.1016/j.fertnstert.2014.10.007.
50. Shridharani A, Owen RC, Elkelany OO, Kim ED. The significance of clinical practice guidelines on adult varicocele detection and management. Asian J Androl 2016;18:269–75. https://doi.org/10.4103/1008-682X.172641.
51. Cayan S, Shavakhabov S, Kadioglu A. Treatment of Palpable Varicocele in Infertile Men: A Meta-analysis to Define the Best Technique. J Androl 2008;30:33–40. https://doi.org/10.2164/jandrol.108.005967.
52. Pagani RL, Ohlander SJ, Niederberger CS. Microsurgical varicocele ligation: surgical methodology and associated outcomes. Fertil Steril 2019;111:415–9. https://doi.org/10.1016/j.fertnstert.2019.01.002.
53. Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev 2012;10. https://doi.org/10.1002/14651858.cd000479.pub5.
54. Kim HJ, Seo JT, Kim KJ, Ahn H, Jeong JY, Kim JH, et al. Clinical significance of subclinical varicocelectomy in male infertility: systematic review and meta-analysis. Andrologia 2016;48:654–61. https://doi.org/10.1111/and.12495.
55. Majzoub A, Sabanegh E. Symptomatic male with subclinical varicocele found on ultrasound evaluation. Asian J Androl 2016; 18:313–4. https://doi.org/10.4103/1008-682X.170864.
56. Kohn TP, Ohlander SJ, Jacob JS, Griffin TM, Lipshultz LI, Pastuszak AW. The Effect of Subclinical Varicocele on Pregnancy Rates and Semen Parameters: a Systematic Review and Meta-Analysis. Curr Urol Rep 2018;19. https://doi.org/10.1007/s11934-018-0798-8.
57. Yamamoto M, Hibi H, Hirata Y, Miyake K, Ishigaki T. Effect of varicocelectomy on sperm parameters and pregnancy rate in patients with subclinical varicocele: a randomized prospective controlled study. J Urol 1996; 155:1636–8.
58. Elbendary MA, Elbadry AM. Right subclinical varicocele: how to manage in infertile patients with clinical left varicocele? Fertil Steril 2009; 92:2050–3. https://doi.org/10.1016/j.fertnstert.2009.05.069.
59. Sun X, Wang J, Peng Y, Gao Q, Song T, Yu W, et al. Bilateral is superior to unilateral varicocelectomy in infertile males with left clinical and right subclinical varicocele: a prospective randomized controlled study. Int Urol Nephrol 2018;50:205–10. https://doi.org/10.1007/s11255-017-1749-x.
60. Stahl P, Schlegel PN. Standardization and documentation of varicocele evaluation. Curr Opin Urol 2011; 21:500–5. https://doi.org/10.1097/MOU.0b013e32834b8698.
61. Choe JH, Seo JT. Is Varicocelectomy Useful for Subfertile Men with Isolated Teratozoospermia? Urology 2015; 86:1123–8. https://doi.org/10.1016/j.urology.2015.08.014.
62. Kirby EW, Wiener LE, Rajanahally S, Crowell K, Coward RM. Undergoing varicocele repair before assisted reproduction improves pregnancy rate and live birth rate in azoospermic and oligospermic men with a varicocele: a systematic review and meta-analysis. Fertil Steril 2016; 106:1338–43. https://doi.org/10.1016/j.fertnstert.2016.07.1093.
63. Aboutaleb HA, Elsherif EA-R, Omar MK, Abdelbaky TM. Testicular Biopsy Histopathology as an Indicator of Successful Restoration of Spermatogenesis after Varicocelectomy in Non-Obstructive Azoospermia. World J Mens Health 2014; 32:43. https://doi.org/10.5534/wjmh.2014.32.1.43.
64. Elbardisi H, El Ansari W, Majzoub A, Arafa M. Does varicocelectomy improve semen in men with azoospermia and clinically palpable varicocele? Andrologia 2020;52 . https://doi.org/10.1111/and.13486.
65. Youssef T, Abd-Elaal E, Gaballah G, Elhanbly S, Eldosoky E. Varicocelectomy in men with nonobstructive azoospermia: Is it beneficial? Int J Surg 2009; 7:356–60. https://doi.org/10.1016/j.ijsu.2009.05.009.
66. Abdel-Meguid TA. Predictors of sperm recovery and azoospermia relapse in men with nonobstructive azoospermia after varicocele repair. J Urol 2012; 187:222–6. https://doi.org/10.1016/j.juro.2011.09.047.
67. Sajadi H, Hosseini J, Farrahi F, Dadkhah F, Sepidarkish M, Sabbaghian M, et al. Varicocelectomy may improve results for sperm retrieval and pregnancy rate in non-obstructive azoospermic men. Int J Fertil Steril 2019; 12:303–5. https://doi.org/10.22074/ijfs.2019.5344.
68. Schlegel PN, Kaufmann J. Role of varicocelectomy in men with nonobstructive azoospermia. Fertil Steril 2004; 81:1585–8. https://doi.org/10.1016/j.fertnstert.2003.10.036.
69. Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial. Eur Urol 2011; 59:455–61. https://doi.org/10.1016/j.eururo.2010.12.008.
70. Majzoub A, Elbardisi H, Arafa M, Agarwal A, Al Said S, Al Rumaihi K. Does the number of veins ligated during varicococele surgery influence post-operative semen and hormone results? Andrology 2016; 4:939–43. https://doi.org/10.1111/andr.12226.
71. Esteves SC, Miyaoka R, Roque M, Agarwal A. Outcome of varicocele repair in men with nonobstructive azoospermia: Systematic review and meta-analysis. Asian J Androl 2016;18:246–53. https://doi.org/10.4103/1008-682X.169562.
72. Weedin JW, Khera M, Lipshultz LI. Varicocele Repair in Patients with Nonobstructive Azoospermia: A Meta-Analysis. J Urol 2010; 183:2309–15. https://doi.org/10.1016/j.juro.2010.02.012.
73. Zhou T, Zhang W, Chen Q, Li L, Cao H, Xu C-L, et al. Effect of varicocelectomy on testis volume and semen parameters in adolescents: a meta-analysis. Asian J Androl 2015; 17:1012. https://doi.org/10.4103/1008-682X.148075.
74. Silay MS, Hoen L, Quadackaers J, Undre S, Bogaert G, Dogan HS, et al. Treatment of Varicocele in Children and Adolescents: A Systematic Review and Meta-analysis from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel (Figure presented.). Eur Urol 2019; 75:448–61. https://doi.org/10.1016/j.eururo.2018.09.042.
75. Locke JA, Noparast M, Afshar K. Treatment of varicocele in children and adolescents: A systematic review and meta-analysis of randomized controlled trials. J Pediatr Urol 2017; 13:437–45. https://doi.org/10.1016/j.jpurol.2017.07.008.
76. Park JH, Pak K, Park NC, Park HJ. How Can We Predict a Successful Outcome after Varicocelectomy in Painful Varicocele Patients? An Updated Meta-Analysis. World J Mens Health 2019;37. https://doi.org/10.5534/wjmh.190112.
77. Jangkhah M, Farrahi F, Sadighi Gilani MA, Hosseini SJ, Dadkhah F, Salmanyazdi R, et al. Effects of Varicocelectomy on Serum Testosterone Levels among Infertile Men with Varicocele. Int J Fertil Steril 2018; 12:169–72. https://doi.org/10.22074/ijfs.2018.5058.
78. Abdel-Meguid TA, Farsi HM, Al-Sayyad A, Tayib A, Mosli HA, Halawani AH. Effects of Varicocele on Serum Testosterone and Changes of Testosterone After Varicocelectomy: A Prospective Controlled Study. Urology 2014; 84:1081–7 . https://doi.org/10.1016/j.urology.2014.05.029.
79. Zaazaa A, Adel A, Fahmy I, Elkhiat Y, Awaad AA, Mostafa T. Effect of varicocelectomy and/or mast cells stabilizer on sperm DNA fragmentation in infertile patients with varicocele. Andrology 2018; 6:146–50. https://doi.org/10.1111/andr.12445.
80. Wang Y-J, Zhang R-Q, Lin Y-J, Zhang R-G, Zhang W-L. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online 2012;25:307–14. https://doi.org/10.1016/j.rbmo.2012.05.002.
81. Abdelbaki SA, Sabry JH, Al-Adl AM, Sabry HH. The impact of coexisting sperm DNAfragmentation and seminal oxidative stress on the outcome of varicocelectomy in infertile patients: A prospective controlled study. Arab J Urol 2017;15:131–9 . https://doi.org/10.1016/j.aju.2017.03.002.
82. Cocuzza M, Alvarenga C, Pagani R. The epidemiology and etiology of perthes’ disease. Osteonecrosis, vol. 68 Suppl 1, Clinics (Sao Paulo); 2014, p. 419–25. https://doi.org/10.1007/978-3-642-35767-1_58.
83. Aduloju OP, Adegun PT. Factors predictive of abnormal semen parameters in male partners of couples attending the infertility clinic of a tertiary hospital in south-western Nigeria. S Afr J Obstet Gynaecol 2016;22:57–61. https://doi.org/10.7196/SAJOG.2016.v22i2.1082.
84. Ahmed A, Bello A, Mbibu N, Maitama H, Kalayi G. Epidemiological and Aetiological Factors of Male Infertility in Northern Nigeria. Niger J Clin Pr 2010;13:205–9.
85. Yeboah ED, Wadhwani JM, Wilson JB. Etiological factors of male infertility in Africa. Int J Fertil n.d.;37:300–7.
86. Wosnitzer M, Goldstein M, Hardy MP. Review of Azoospermia. Spermatogenesis 2014; 4:e28218. https://doi.org/10.4161/spmg.28218.
87. Patel AS, Leong JY, Ramasamy R. Prediction of male infertility by the World Health Organization laboratory manual for assessment of semen analysis: A systematic review. Arab J Urol 2018; 16:96–102. https://doi.org/10.1016/j.aju.2017.10.005.
88. Aziz N. The Importance of Semen Analysis in the Context of Azoospermia. Clinics 2013; 68 Suppl1.
89. Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European association of urology guidelines on male infertility: The 2012 update. Eur Urol 2012; 62:324–32. https://doi.org/10.1016/j.eururo.2012.04.048.
90. European Association of Urology. EAU Guidelines: Male Infertility | Uroweb n.d. https://uroweb.org/guideline/male-infertility/ (accessed May 19, 2020).
91. Jarvi K, Lo K, Fischer A, Grantmyre J, Zini A, Chow V, et al. CUA guideline: The workup of azoospermic males. J Can Urol Assoc 2010; 4:163–7. https://doi.org/10.5489/cuaj.10050.
92. Yu J, Chen Z, Ni Y, Li Z. CFTR mutations in men with congenital bilateral absence of the vas deferens (CBAVD): a systemic review and meta-analysis. Hum Reprod 2011;27:25–35. https://doi.org/10.1093/humrep/der377.
93. American Urological Association. The Evaluation of the Azoospermic Male - American Urological Association n.d. https://www.auanet.org/guidelines/azoospermic-male-best-practice-statement (accessed May 19, 2020).
94. Bernie AM, Mata DA, Ramasamy R, Schlegel PN. Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: A systematic review and meta-analysis. Fertil Steril 2015; 104:1099-1103.e3. https://doi.org/10.1016/j.fertnstert.2015.07.1136.
95. Corona G, Minhas S, Giwercman A, Bettocchi C, Dinkelman-Smit M, Dohle G, et al. Sperm recovery and ICSI outcomes in men with non-obstructive azoospermia: a systematic review and meta-analysis. Hum Reprod Update 2019; 25:733–57. https://doi.org/10.1093/humupd/dmz028.
96. Kalsi JS, Shah P, Thum Y, Muneer A, Ralph DJ, Minhas S. Salvage micro-dissection testicular sperm extraction; Outcome in men with non-obstructive azoospermia with previous failed sperm retrievals. BJU Int 2015; 116:460–5. https://doi.org/10.1111/bju.12932.
97. Donoso P, Tournaye H, Devroey P. Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum Reprod Update 2007; 13:539–49. https://doi.org/10.1093/humupd/dmm029.
98. Deruyver Y, Vanderschueren D, Van der Aa F. Outcome of microdissection TESE compared with conventional TESE in non-obstructive azoospermia: A systematic review. Andrology 2014;2:20–4. https://doi.org/10.1111/j.2047-2927.2013.00148.x.
99. Yu Z, Wei Z, Yang J, Wang T, Jiang H, Li H, et al. Comparison of intracytoplasmic sperm injection outcome with fresh versus frozen-thawed testicular sperm in men with nonobstructive azoospermia: a systematic review and meta-analysis. J Assist Reprod Genet 2018;35:1247–57. https://doi.org/10.1007/s10815-018-1206-5.
100. Santi, D., et al. FSH treatment of male idiopathic infertility improves pregnancy rate: A metaanalysis. Endocrine Connect, 2015. 4: R46. https://pubmed.ncbi.nlm.nih.gov/261135211.
101. American Urological Association. The Management of Obstructive Azoospermia - American Urological Association n.d. https://www.auanet.org/guidelines/obstructive-azoospermia-best-practice-statement (accessed May 19, 2020).
102. Avellino GJ, Lipshultz LI, Sigman M, Hwang K. Transurethral resection of the ejaculatory ducts: etiology of obstruction and surgical treatment options. Fertil Steril 2019; 111:427–43. https://doi.org/10.1016/j.fertnstert.2019.01.001.
103. Jeong SC, Lee S, Ku JY, Lee SD. Clinical Characteristics and Treatment of Cryptorchidism in Adults: A Single Center Experience. World J Mens Health 2014; 32:110. https://doi.org/10.5534/wjmh.2014.32.2.110.
104. Rogers E, Teahan S, Gallagher H, Butler MR, Grainger R, McDermott TE, et al. The role of orchiectomy in the management of postpubertal cryptorchidism. J Urol 1998; 159:851–4.
105. Grasso M, Buonaguidi A, Lania C, Bergamaschi F, Castelli M, Rigatti P. Postpubertal Cryptorchidism: Review and Evaluation of the Fertility. Eur Urol 1991; 20:126–8. https://doi.org/10.1159/000471680.
106. Lin YM, Hsu CC, Wu MH, Lin JSN. Successful testicular sperm extraction and paternity in an azoospermic man after bilateral postpubertal orchiopexy. Urology 2001; 57:365. https://doi.org/10.1016/S0090-4295 (00)01006-2.
107. Matsushita K, Yamaguchi K, Li F, Okada K, Ando M, Chiba K, et al. Achieved pregnancy with the delivery of a healthy child by TESE-ICSI 7 years after bilateral adult orchidopexy: a case report. Andrologia 2014; 46:948–50. https://doi.org/10.1111/and.12174.
108. RAMAN JD, SCHLEGEL PN. Testicular Sperm Extraction with Intracytoplasmic Sperm Injection is Successful for the Treatment of Nonobstructive Azoospermia Associated with Cryptorchidism. J Urol 2003; 170:1287–90. https://doi.org/10.1097/01.ju.0000080707.75753.ec.
109. Chung JM, Lee SD. Individualized Treatment Guidelines for Postpubertal Cryptorchidism. World J Mens Health 2015; 33:161. https://doi.org/10.5534/wjmh.2015.33.3.161.
110. Kim ED, Crosnoe L, Bar-Chama N, Khera M, Lipshultz LI. The treatment of hypogonadism in men of reproductive age. Fertil Steril 2013; 99:718–24. https://doi.org/10.1016/j.fertnstert.2012.10.052.
111. Dohle GR, Arver S, Bettocchi C, Jones TH, Kliesch S. EAU Guidelines: Male Hypogonadism | Uroweb n.d. https://uroweb.org/guideline/male-hypogonadism/ (accessed June 6, 2020).
112. Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and Management of Testosterone Deficiency: AUA Guideline. J Urol 2018; 200:423–32. https://doi.org/10.1016/j.juro.2018.03.115.
113. Hackett G, Kirby M, Edwards D, Jones TH, Wylie K, Ossei-Gerning N, et al. British Society for Sexual Medicine Guidelines on Adult Testosterone Deficiency, With Statements for UK Practice. J Sex Med 2017;14:1504–23. https://doi.org/10.1016/j.jsxm.2017.10.067.
114. Goodman N, Guay A, Dandona P, Dhindsa S, Faiman C, Cunningham GR. American association of clinical endocrinologists and American college of endocrinology position statement on the association of testosterone and cardiovascular risk. Endocr Pract 2015;21:1066–73. https://doi.org/10.4158/EP14434.PS.
115. Khera M, Adaikan G, Buvat J, Carrier S, El-Meliegy A, Hatzimouratidis K, et al. Diagnosis and Treatment of Testosterone Deficiency: Recommendations From the Fourth International Consultation for Sexual Medicine (ICSM 2015). J Sex Med 2016; 13:1787–804. https://doi.org/10.1016/j.jsxm.2016.10.009.
116. Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone Therapy in Men with Hypogonadism: An Endocrine Society. J Clin Endocrinol Metab 2018; 103:1715–44. https://doi.org/10.1210/jc.2018-00229.
117. Ho CCK, Tan HM. Treatment of the Hypogonadal Infertile Male—A Review. Sex Med Rev 2013; 1:42–9. https://doi.org/10.1002/smrj.4.
118. Salter CA, Mulhall JP. Guideline of guidelines: testosterone therapy for testosterone deficiency. BJU Int 2019; 124:722–9. https://doi.org/10.1111/bju.14899.
119. Ahmed K, Hatzimouratidis K, Muneer A. Male Sexual Dysfunction and Hypogonadism Guidelines for the Aging Male. Eur Urol Focus 2017; 3:514–6. https://doi.org/10.1016/j.euf.2017.12.004.
120. Sykiotis GP, Hoang X-H, Avbelj M, Hayes FJ, Thambundit A, Dwyer A, et al. Congenital Idiopathic Hypogonadotropic Hypogonadism: Evidence of Defects in the Hypothalamus, Pituitary, and Testes. J Clin Endocrinol Metab 2010; 95:3019–27. https://doi.org/10.1210/jc.2009-2582.
121. Rohayem J, Hauffa BP, Zacharin M, Kliesch S, Zitzmann M. Testicular growth and spermatogenesis: new goals for pubertal hormone replacement in boys with hypogonadotropic hypogonadism? -a multicentre prospective study of hCG/rFSH treatment outcomes during adolescence-. Clin Endocrinol (Oxf) 2017; 86:75–87. https://doi.org/10.1111/cen.13164.
122. Wiehle RD, Fontenot GK, Wike J, Hsu K, Nydell J, Lipshultz L. Enclomiphene citrate stimulates testosterone production while preventing oligospermia: a randomized phase II clinical trial comparing topical testosterone. Fertil Steril 2014;102:720–7. https://doi.org/10.1016/j.fertnstert.2014.06.004.
123. Rambhatla A, Mills JN, Rajfer J. The Role of Estrogen Modulators in Male Hypogonadism and Infertility. Rev Urol 2016; 18:66–72. https://doi.org/10.3909/riu0711.
124. Çakan M, Aldemir M, Topcuoglu M, Altuğ U. Role of Testosterone/Estradiol Ratio in Predicting the Efficacy of Tamoxifen Citrate Treatment in Idiopathic Oligoasthenoteratozoospermic Men. Urol Int 2009; 83:446–51. https://doi.org/10.1159/000251186.
125. Cocuzza M, Agarwal A. Nonsurgical treatment of male infertility: specific and empiric therapy. Biologics 2007; 1:259–69.
126. MENG M V., GREENE KL, TUREK PJ. SURGERY OR ASSISTED REPRODUCTION? A DECISION ANALYSIS OF TREATMENT COSTS IN MALE INFERTILITY. J Urol 2005; 174:1926–31. https://doi.org/10.1097/01.ju.0000176736.74328.1a.
127. Sigman M. Empiric and lifestyle therapies for male infertility—should we recommend them? Fertil Steril 2020; 113:1120. https://doi.org/10.1016/j.fertnstert.2020.04.014.
128. Öztekin Ü, Caniklioğlu M, Sarı S, Selmi V, Gürel A, Işıkay L. Evaluation of Male Infertility Prevalence with Clinical Outcomes in Middle Anatolian Region. Cureus 2019. https://doi.org/10.7759/cureus.5122.
129. Devroey P, Fauser BCJM, Diedrich K. Approaches to improve the diagnosis and management of infertility. Hum Reprod Update 2009; 15:391–408. https://doi.org/10.1093/humupd/dmp012.
130. Kandavel V, Cheong Y. Does intra-uterine insemination have a place in modern ART practice? Best Pract Res Clin Obstet Gynaecol 2018; 53:3–10. https://doi.org/10.1016/j.bpobgyn.2018.08.003.
131. Goverde AJ, McDonnell J, Vermeiden JP, Schats R, Rutten FF, Schoemaker J. Intrauterine insemination or in-vitro fertilisation in idiopathic subfertility and male subfertility: a randomised trial and cost-effectiveness analysis. Lancet 2000; 355:13–8. https://doi.org/10.1016/S0140-6736 (99)04002-7.
132. Tournaye H. Male factor infertility and ART. Asian J Androl 2012; 14:103–8. https://doi.org/10.1038/aja.2011.65.
133. Huang LN, Tan J, Hitkari J, Dahan MH. Should IVF be used as first-line treatment or as a last resort? A debate presented at the 2013 Canadian Fertility and Andrology Society meeting. Reprod Biomed Online 2015; 30:128–36. https://doi.org/10.1016/j.rbmo.2014.10.004.
134. Reindollar RH, Regan MM, Neumann PJ, Levine B-S, Thornton KL, Alper MM, et al. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril 2010; 94:888–99. https://doi.org/10.1016/j.fertnstert.2009.04.022.
135. Smith LK, Phy JL, Dorsett MJO. Treatment of mild/moderate male factor infertility with in vitro fertilization (IVF) instead of intracytoplasmic sperm injection (ICSI): a ten-year retrospective analysis. Fertil Steril 2007; 88:S116–7. https://doi.org/10.1016/j.fertnstert.2007.07.376.
136. Schlegel PN, Girardi SK. In Vitro Fertilization for Male Factor Infertility. J Clin Endocrinol Metab 1997; 82:709–16. https://doi.org/10.1210/jcem.82.3.3785.
137. Palermo G, Joris H, Devroey P, Steirteghem A Van. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 1992; 340:17–8. https://doi.org/10.1016/0140-6736 (92)92425-F.
138. Palermo GD, Cohen J, Alikani M, Adler A, Rosenwaks Z. Intracytoplasmic sperm injection: a novel treatment for all forms of male factor infertility. Fertil Steril 1995; 63:1231–40. https://doi.org/10.1016/s0015-0282 (16)57603-1.
139. Tannus S, Son W-Y, Gilman A, Younes G, Shavit T, Dahan M-H. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod 2016. https://doi.org/10.1093/humrep/dew298.
140. Hamberger L, Lundin K, Sjogren A, Soderlund B. Indications for intracytoplasmic sperm injection. Hum Reprod 1998; 13:128–33. https://doi.org/10.1093/humrep/13.suppl_1.128.
141. Nikolettos N, Al-Hasani S, Baukloh V, Schöpper B, Demirel LC, Baban N, et al. The outcome of intracytoplasmic sperm injection in patients with retrograde ejaculation. Hum Reprod 1999; 14:2293–6. https://doi.org/10.1093/humrep/14.9.2293.
142. Rubino P, Viganò P, Luddi A, Piomboni P. The ICSI procedure from past to future: a systematic review of the more controversial aspects. Hum Reprod Update 2015:dmv050. https://doi.org/10.1093/humupd/dmv050.
143. Chavez-Badiola A, Drakeley AJ, Finney V, Sajjad Y, Lewis-Jones DI. Necrospermia, antisperm antibodies, and vasectomy. Fertil Steril 2008; 89:723.e5-723.e7. https://doi.org/10.1016/j.fertnstert.2007.04.007.
144. Dumont A, Barbotin A-L, Lefebvre-Khalil V, Mitchell V, Rigot J-M, Boitrelle F, et al. La necrozoospermie : du diagnostic étiologique à la prise en charge thérapeutique. Gynécologie Obs Fertil Sénologie 2017; 45:238–48. https://doi.org/10.1016/j.gofs.2017.01.010.
a. L. Check, J. H. Check DK. ICSI AS AN EFFECTIVE THERAPY FOR MALE FACTOR WITH ANTISPERM ANTIBODIES. Arch Androl 2000; 45:125–30. https://doi.org/10.1080/01485010050193887.
145. Nagy ZP, Verheyen G, Liu J, Joris H, Janssenswillen C, Wisanto A, et al. Andrology: Results of 55 intracytoplasmic sperm injection cycles in the treatment of male-immunological infertility. Hum Reprod 1995; 10:1775–80. https://doi.org/10.1093/oxfordjournals.humrep.a136172.
146. Palermo GD, Neri Q V., Schlegel PN, Rosenwaks Z. Intracytoplasmic Sperm Injection (ICSI) in Extreme Cases of Male Infertility. PLoS One 2014; 9:e113671. https://doi.org/10.1371/journal.pone.0113671.
147. Kang Y-N, Hsiao Y-W, Chen C-Y, Wu C-C. Testicular sperm is superior to ejaculated sperm for ICSI in cryptozoospermia: An update systematic review and meta-analysis. Sci Rep 2018; 8:7874. https://doi.org/10.1038/s41598-018-26280-0.
148. Ku F-Y, Wu C-C, Hsiao Y-W, Kang Y-N. Association of sperm source with miscarriage and take-home baby after ICSI in cryptozoospermia: a meta-analysis of testicular and ejaculated sperm. Andrology 2018; 6:882–9. https://doi.org/10.1111/andr.12546.
149. Tahmasbpour E, Balasubramanian D, Agarwal A. A multi-faceted approach to understanding male infertility: gene mutations, molecular defects and assisted reproductive techniques (ART). J Assist Reprod Genet 2014; 31:1115–37. https://doi.org/10.1007/s10815-014-0280-6.
150. Varga K, Tóth N, Bogár ÉB, Csontos L, Szabó K, Debreceni D, et al. The demise of preimplantation genetic testing for aneuploidy (PGT-A) in Hungary and its effect on patient care. Eur J Med Genet 2019; 62:103669. https://doi.org/10.1016/j.ejmg.2019.05.008.
151. Gianaroli L, Munné S, Magli MC, Ferraretti AP. Preimplantation genetic diagnosis of aneuploidy and male infertility. Int J Androl 1997; 20 Suppl 3:31–4.
152. Mazzilli R, Cimadomo D, Vaiarelli A, Capalbo A, Dovere L, Alviggi E, et al. Effect of the male factor on the clinical outcome of intracytoplasmic sperm injection combined with preimplantation aneuploidy testing: observational longitudinal cohort study of 1,219 consecutive cycles. Fertil Steril 2017; 108:961-972.e3. https://doi.org/10.1016/j.fertnstert.2017.08.033.
153. Dul EC, van Echten-Arends J, Groen H, Dijkhuizen T, Land JA, van Ravenswaaij-Arts CMA. Chromosomal abnormalities in azoospermic and non-azoospermic infertile men: numbers needed to be screened to prevent adverse pregnancy outcomes. Hum Reprod 2012; 27:2850–6. https://doi.org/10.1093/humrep/des222.
154. Barratt CLR, Björndahl L, De Jonge CJ, Lamb DJ, Osorio Martini F, McLachlan R, et al. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance—challenges and future research opportunities. Hum Reprod Update 2017; 23:660–80. https://doi.org/10.1093/humupd/dmx021.
